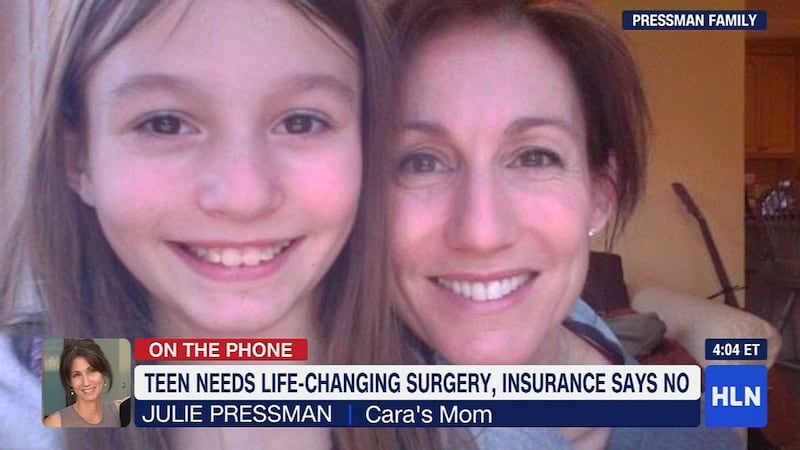
ROCKLAND. N.Y. — A New York teenager had strong words when her parents’ insurance company denied her coverage for minimally invasive brain surgery that could end the seizures that have plagued her since she was 9.
The surgery for Cara Pressman, 15, was rejected by Aetna six weeks ago, CNN reported. She had been scheduled to have laser ablation surgery on Oct. 23, but three days before the procedure her family received a rejection letter from the insurance giant.
TRENDING NOW:
- WATCH: Injured Shazier celebrates Steelers' win in hospital
- Explosion reported near the Port Authority in New York
- WATCH: Seahawks' Quinton Jefferson tries to climb into stands after fans throw concessions
- VIDEO: 2018 Golden Globe Awards Nominees
“When my parents told me, I went kind of blank and started crying,” Cara said. “I cried for like an hour.”
Since then, the teen from Rockland, New York, has suffered more than two dozen seizures.
“Considering they're denying me getting surgery and stopping this thing that's wrong with my brain, I would probably just say, ‘Screw you.’” Cara told CNN.
Cara’s seizures can be triggered by stress, by being happy, by exerting herself -- almost anything. “It's like having a nightmare but while you're awake," she told CNN.
Aetna is the third-largest health insurance provider in the country, providing medical coverage to 23.1 million people.
Neurologists consider laser ablation, which is performed through a small hole in the skull, to be safer and more precise than traditional brain surgery, CNN reported.
In its rejection letter, Aetna said it considered laser ablation surgery “experimental and investigational for the treatment of epilepsy because the effectiveness of this approach has not been established.”
"Clinical studies have not proven that this procedures (sic) effective for treatment of the member's condition," Aetna wrote.
The insurance company did approve Cara for the more invasive and more expensive open brain surgery, CNN reported.
Dr. Jamie Van Gompel, a neurosurgeon at the Mayo Clinic, said Aetna's assessment was wrong.
“I would not call it experimental at all,” Van Gompel told CNN. “It's definitely not an experimental procedure. There've been thousands of patients treated with it. It's FDA (Food and Drug Administration)-approved. There's a lot of data out there to suggest it's effective for epilepsy."
When pressed for a better explanation on its denial, Aetna stood by its rejection, saying it was in the best interest of the patients, CNN reported, noting that the insurance company’s tone had softened somewhat.
“Clinical effectiveness and our members' safety are the primary criteria we use in determining whether a treatment or service is medically necessary,” Aetna told CNN. “There is currently a limited amount of evidence-based, clinical studies related to laser ablation surgery. As noted by the Epilepsy Foundation, only studies with a very small number of participants have been used to report the effectiveness of this procedure. We consistently evaluate any new studies or additional evidence when developing our clinical policy bulletins, and will continue to do so for this procedure.”
The Epilepsy Foundation strongly objected to Aetna's remarks, saying the insurance company took its information out of context, CNN reported.
Laser ablation surgery "has emerged as a new minimally invasive surgical option that is best suited for patients with symptomatic localization-related epilepsy," said Dr. Jacqueline French, the chief science officer with the Epilepsy Foundation.
Meanwhile, the Pressman family is frustrated, knowing that a procedure is available to Cara but unobtainable through its insurance.
“It's just so frustrating for us to know there's a solution out there -- a way to fix our daughter -- and some bureaucratic machine is preventing this from happening,” said Robert Pressman, Cara’s father. “You get so angry, but you don't know who to take it out on, because there's no particular person that's doing it. It's this big bureaucracy that's preventing this from happening.”
Robert Pressman and his wife, Julie, said they have paid $24,000 for insurance with Aetna this year. They said they are determined to get Cara laser ablation surgery with or without the insurance company's help. They will appeal Aetna's latest rejection -- but are not optimistic.
To prepare, they are considering dipping into their retirement funds to pay the $300,000 out of pocket, CNN reported.
“Cara is worth every penny, but man,” Julie Pressman said. “‘Screw Aetna,’ indeed, to quote my kid.”
Cox Media Group